Finally, MRI and Radiation Therapy get together to fight Cancer like never before
Learn about Adaptive MR Image-Guided Radiotherapy, a cutting-edge technology combining MRI and radiation therapy to increase cancer treatment precision.
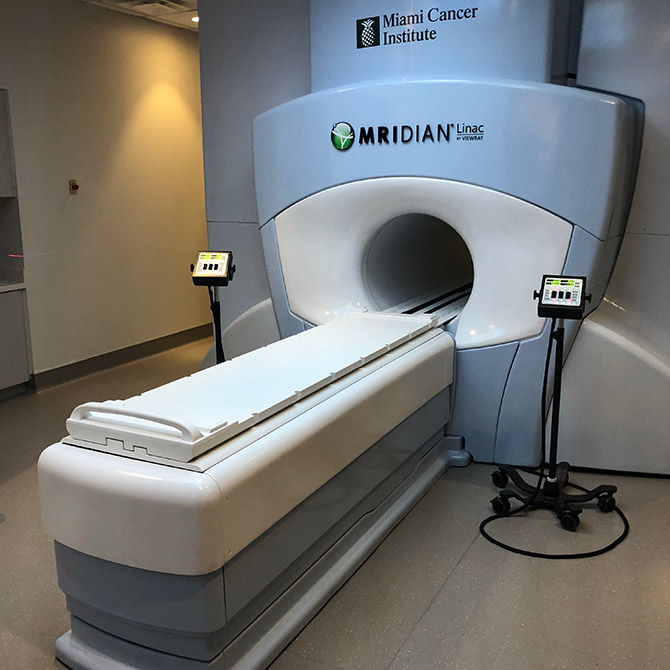
Cancer treatment has come a long way. Treatments that were once thought of as science fiction, today, are science fact. Recently, I saw a presentation at the Miami Cancer Institute where they were showing one of their latest technologies for fighting cancer and I have to say, I was pretty impressed.
The technology is called Adaptive MR Image-Guided Radiotherapy. Like all medical terms, it sounds as complicated as possible, I guess doctors are used to the complicated names but, for us normal people, it takes a little more explanation as to what it means. Let’s start with the basics.
This fancy name is the combination of two very well-established technologies. Magnetic Resonance Imaging (MRI) and Radiation Therapy. MRIs have been in use for a long time. It uses a combination of radio waves and magnets to create a high-resolution image inside the patient’s body. A common misconception is that MRIs use radiation and that’s not the case. On the other hand, external radiation therapy has been in use for a long time as well. In that case, a machine delivers a beam of high-energy particles to destroy or damage the tumor cells, so they can’t replicate.
Each technology by itself is pretty well established but, this is the first time that both of them are combined in one single machine called MRIdian, manufactured by a company called ViewRay.
So, what’s the big deal?
When it comes to cancer treatment, each person’s diagnosis is unique but there are some common traits that we all share. For example, some parts of the body stay still, like the brain, so radiation treatment is technically easier since doctors can have a scan of the tumor and target the exact area more precisely and aggressively.
In other parts of the body, like the abdomen, it’s not so easy because it’s constantly moving. How much? Check out this picture of the difference in position in just 5 days.
You may say, well, 5 days is a long time, so they could technically take an image of the tumor the same day and this wouldn’t be a problem, right? Not so fast.
For example, when targeting pancreatic cancer with radiation, the patient’s breathing and the constant intestinal motion create a moving target. The pancreas moves, or the intestines can get in the way of the radiation beam and as you can imagine, this is not ideal. That’s why traditional radiation therapy, where you have a static image previously taken, is not very precise. What are the consequences?
As you can imagine, in abundance of care, doctors would not use higher doses of radiation in fear of causing toxicity, which is a doctor’s term for radiating healthy surrounding tissues and organs.
If I’m going to use an analogy, imagine going to a shooting range where one day you take a look at the bulls eye, aim and are ready to fire, then you come back another day and have to take the shot but now, with your eyes covered.
What changes with the MRIdian?
With this new machine, doctors can see an image in real time of the location and of the tumor clearly delineated. This allows them to differentiate it from surrounding healthy tissues and organs that way, they can more precisely administer radiation and in some cases, even use higher doses to fight the cancer more aggressively. This allows them also to have a treatment plan that better adapts to the conditions of the patient at the very moment.
https://vimeo.com/205920769
This is the first and only FDA-cleared treatment of this kind and so far has shown promising results in the treatment of pancreatic cancer. It’s impressive that these two advanced technologies can be successfully combined to increase the precision of treatment for cancer patients.


